A History of Heart Rate & Pulse Oximetry
- V. A. Cyr
- Sep 4, 2024
- 12 min read
Updated: Oct 9, 2024
Our next vital sign to examine is Heart Rate or Pulse. Since we will examine pulse, we will also look into Pulse Oximetry. Everyone has felt their pulse at one point. What is an oximetre? How does a machine on your finger tell you so much about your health? This post will examine the history behind these techniques that nurses use every day and explain why they are so crucial in an assessment!
Definitions & Types
Heart Rate
Heart rate (pulse or heartbeat) is the number of times the heart beats in one minute (beats per minute or bpm). Pulse comes from the Latin word pulsus, meaning “to beat” (Merriam-Webster, n.d.). This can be counted manually or automatically with a vital signs machine. If done manually, the nurse will palpate a vein or artery or auscultate the heart to count the number of beats. Many blood vessels, like the radial, femoral, and jugular veins, can be used to find a pulse. Please read the post on Auscultation for the locations to auscultate the heart. If done with a machine, it can be calculated with a blood pressure monitor, a pulse oximetre (see below), or an electrocardiogram (ECG).

A diagram of manual pulse measurement on the radial vein of the left arm (Cosinuss, n.d.).

Here is an example of an ECG machine placed on a patient (Mount Sinai, 2024). More information on ECGs can be found at A History of ECGs.
Physiology of the Heart
The heart’s anatomy is reviewed in the Auscultation post. Here, we will review the physiology, or how the heart beats. Heart rate is controlled by electricity through the cardiac conduction system. The electrical signal passes from the top to the bottom of the heart, causing the heart muscles to contract and pump blood.

This is a diagram of the heart’s electrical conduction system (Klabunde, 2023).
The signal originates in the medulla in the brainstem, which regulates all essential body functions (e.g., heart rate, breathing, oxygen levels). The electrical signal from the brain goes to the pacemaker cells located in the sinoatrial node (SAN on the diagram). The signal goes through the right and left atria (RA and LA), causing the blood to be pumped into the right and left ventricles (RV and LV). The electrical signal then reaches pacemaker cells in the atrioventricular node (AVN), as seen with the green arrows in the diagram above. The AVN slows the signal, allowing the ventricles to fill with blood. The AVN then sends another signal that travels down the ventricles (RV and LV), causing them to contract and pump blood into the body (NHLBI, 2022).
Factors Affecting Heart Rate
Age
Usually, as a person ages, their heart rate decreases throughout their life. Most adults stay between 60 to 100 bpm, except some elite athletes. However, children start with high heart rates, then gradually decrease until they reach the average adult range (usually during adolescence).

Here is a table indicating the acreage range of heart rate in children of different ages (Plaza, 2023).
Activity
Living a sedentary life and being obese can contribute to heart disorders and heart rate variability (Peterson, 2007). Drinking caffeine can increase the pulse by making the heart beat faster, making it feel like you have more energy or anxious. This is why high levels of caffeine can cause heart problems. Also, pulse variability tends to be higher when sleeping than when awake (King, 2024).
Lifestyle
Habits such as drinking alcohol and smoking will increase the risk of heart disease. A stressful occupation exposes a person to particulates, chemicals, electromagnetic fields, vibrating tools, long working hours, shift work (overnights), and fatigue, affecting their heart (Tarnoki et al., 2021).
Medications
Tachycardia can be induced by drugs such as antibiotics and antidepressants. Medications for hypertension (e.g., beta-blockers) will lower blood pressure, which can also decrease the heart rate. Sedatives used in surgical procedures (e.g., propofol) can also reduce the pulse and must be monitored.
Comorbidities
Conditions like anemia (low hemoglobin), anxiety, and depression all affect the heart and pulse (Peterson, 2007). Patients with heart disease (e.g., hypertension), metabolic disease (e.g., diabetes), lung disease (COPD), and kidney disease (chronic kidney insufficiency) all cause lower pulse rates than the average for their age group and sex (King, 2024).
Pulse Oximetry
Pulse oximetry is considered the fifth vital sign (after pulse, blood pressure, temperature, and respirations). Spectrophotometry technique using the Beer-Lambert Law measures blood oxygen saturation (SpO2) (Torp et al., 2023). It is a technique for measuring blood oxygen levels by shining a light with a specific wavelength through tissue (Torp et al., 2023).

Diagram of how the light penetrates the skin and detects the oxygen saturation (Mendelson, 2017).
This is done with a machine called a pulse oximetre. Usually done on the fingernails, it can also be measured on the toes and earlobes. Ozimetres also come in one-time-use adhesive probes (i.e., newborns). It is measured in percentages, with 100% being optimal. The usual range of an average healthy person is between 95 to 100%. People living in higher elevation areas may have a lower blood oxygen level (Torp et al., 2023).

Here is an example of a modern portable pulse oximetre (London Drugs, n.d.).

Here are two examples of adhesive oximetre sensors: one for the finger or toe and one for the newborn foot (Tri-anim, n.d.).
Photoplethysmograph
A photoplethsmograph (PPG or "pleth") is a graphic display of the pulse oximetre signals received from the sensor (Jubran, 2015). On a vital sign machine, there are waveforms to show the ECG tracing, pulse (from the ECG), oxygen saturation (SpO2), and respirations (CO2). The waveform for pulse oximetry can differ depending if there are artifacts (signals that distract the sensor). The various pulse tracings will be covdred in a future post.

Here is a vital signs machine with waveform tracings that can be printed out on a paper (India Mart, n.d.). The ECG tracing in is green, oxygen saturation in blue, respirations in yelllow (with blood pressure in red and temperature also in green).

These are examples of waveforms that can be seen from an oximetre and the artifacts that cause them (Jubran, 2015). Low perfusion could indicate a weak pulse or other factors (see below). Noise and motion artifacts can occur if the patient is moving too much or if the practioner is interfering with the signal somehow.
Factors Affecting Pulse Oximetry
Comorbidities
Any condition that decreases blood perfusion to the tissues can cause a low saturation level. Respiratory symptoms like dyspnea (shortness of breath), tachypnea (breathing too fast), and bradypnea (breathing too slow) can all contribute to a low oxygen level in the blood. Disorders like anemia can also decrease the oxygen level as insufficient hemoglobin is distributed in the blood. Any condition that causes someone to have more carbon dioxide (CO2) in the body, like sleep apnea and cigarette smoking, will decrease the saturation levels.
Oximetre-Specific Factors
Pulse oximetry can be challenging in colder temperatures (Torp et al., 2023). This occurs because when the temperature is too cold, the body will conserve blood for the essential organs (i.e., heart and brain) by reducing peripheral blood flow. This is also why fingers and toes feel so much colder in winter. Oximetres also have difficulty measuring saturation through dark-coloured nail polish (black or blue) or artificial fingernails (Torp et al., 2023). (This is why the nurse might ask you to remove your nail polish before a procedure!)
Origins
Heart Rate
There has been mention of heart rate or pulse (e.g., heart “speed” or tachycardia) as early as texts from ancient Greek times. The first illustration of a doctor measuring a pulse was in Aldebrande de Florence's “Traité de Medecine” in 1356 (Ceconi et al., 2011). In 1628, William Harvey found through research that the heart expels more blood in one hour than the man’s weight (Ceconi et al., 2011). Therefore, Harvey calculated that his heart must beat at least 60 times per minute to pump this much blood through the body.
1707 saw the invention of the “physician pulse watch” by Doctor Floyer and watchmaker Watson (Billman, 2011). The second hand can be stopped in this particular watch to aid in counting the heart rate accurately.
Research began into the various effects of the heart rate. In 1733, Hales found that a person’s respiration rate (breathing) can affect their heart rate (Billman, 2011). Ludwig furthered this research finding in 1847 and found respiratory sinus arrhythmia (change in heart rate from respirations) (Billman, 2011). In the 1960s, heart rate variability (HRV) became the focus of many research projects (Billman, 2011). HRV is the phenomenon of variation in the time interval between heartbeats.
The wireless ECG, made by Polar in 1977, became popularized and used in high-endurance athletes (Wikipedia, 2024). Then, Polar released the first watch with the ability to count a person’s pulse in 1982. In the 1990s and 2000s, more recent devices have used optics to measure heart rate by shining light from an LED through the skin and measuring how it scatters off blood vessels (Wikipedia, 2024). This is the same technique used to measure pulse oximetry. This is very popular today in fitness monitors, and some more advanced models can detect HRV (Wikipedia, 2024).
Timeline Throughout History: Pulse Measurement

Pulse Oximetry
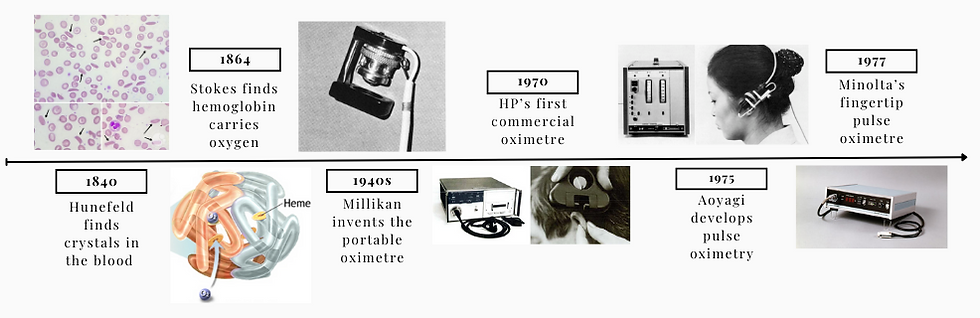
The research on pulse oximetry goes back to the beginnings of understanding the blood. In 1840, Friedrich Hunefeld found “crystals” while looking at the blood through a microscope (Cable and Sensors, n.d.). In 1864, Stokes discovered that these “crystals” are hemoglobin and what binds oxygen in the blood to carry it around the body (Cable and Sensors, n.d.).
Karl Matthes used two waves of light in 1935 to measure the oxygen in the blood.
The first portable oximetre was made by Glenn Millikan in the 1940s (Cable and Sensors, n.d.). These were used on World War II pilots to ensure they were getting enough oxygen while flying at high altitudes.
Around 1948, Earl Wood invented an oximetre for the ear (Cable and Sensors, n.d.). This machine used pneumatic pressure to squeeze the blood in the ear for better measurement.
Robert Shaw conducted research in 1964 on using more wavelengths of light in the sensor to improve the reading (Cable and Sensors, n.d.). Then, Hewlett Packard (HP) unveiled the first commercial ear oximetre in 1970, including eight wavelengths (Cable and Sensors, n.d.).
Takuo Aoyagi invented the first pulse oximetre between 1972 and 1974. This tool was also used on the ear but worked more similarly to the modern-day pulse oximetres. Finally, the Minolta company launched the first fingertip pulse oximetre (Cable and Sensors, n.d.). The 1980s had a surge in technology that allowed for better semiconductors to be produced by Biox Technology and Nellcor (Cable and Sensors, n.d.). The modern pulse oximetre probes use this technology (see the diagram above).
Timeline Throughout Hisotry: Oximetry Measurement
Uses in Medicine
Heart Rate
When assessing heart rate, it is measured (in bpm) and described based on its rhythm (regular or irregular) and strength (strong, weak or bounding) (Pickering, 2013). It is usually counted for 30 seconds and doubled to get the number of beats per minute. However, if the pulse is irregular, the medical professional should be counting for an entire minute. Also, the heart rate needs to be monitored while administering certain medications. For example, before giving Digoxin (medication to treat congestive heart failure), the nurse should auscultate the heart for one minute to assess for abnormalities before administration.
Normal Pulse Findings
At rest, a regular pulse for an adult is between 60 to 100 bpm, regular, and strong.
A strong pulse is easily felt through the skin during palpation.
Regular pulse rhythm is a heart rate that does not vary in length and consistency. There are no extra short or long pauses between the beats, meaning each beat is the same.
Abnormal Pulse Findings
Tachycardia is the heart beating too fast (tachy), over 120 bpm. This is common when exercising but can be detrimental in cases of people with disorders (e.g., chronic anxiety).
Bradycardia occurs when the heart beats too slowly (brady), at less than 60 bpm. However, a heart rate of 40 to 60 bpm can be a regular finding in high-endurance athletes (e.g., runners or cyclists).
Pulse strengths that are weak (difficulty palpating pulse) or bounding (“exploding” through the skin) are not typical. These can be indicative of disorders (e.g., anxiety, dehydration) or ageing (elderly have weaker pulses).
Irregular pulse rhythm can indicate a cardiac arrhythmia. Arrhythmias are any differences in the heart rate, like extra beats or changes in timings. Some examples of arrhythmias are atrial fibrillation, ventricular tachycardia, or heart block. These will be further discussed in a future post.
Conduction disorders occur when the heart’s electrical signals are not generated or travel through the heart properly. These are known as heart blocks, a type of arrhythmia.
Here is a video comparing a regular heart rate, bradycardia and tachycardia (Radiology Buzz, 2020).
Pulse Oximetry
Normal Oximetry Findings
A healthy person will have an oxygen saturation of between 95% and 100%.
People with respiratory disorders (see below) will have lower levels (between 88% and 92%). If the person’s oxygen is too high in their blood, the brain will not tell them to take a breath, as it thinks it does not need oxygen then.
Abnormal Oximetry Findings
Hypoxemia is low (hypo) blood (emia) oxygen (ox) and is a sign of an underlying illness, either blood- or respiration-related (Mayo Clinic, 2023). If untreated with supplemental oxygen, hypoxemia can lead to hypoxia.
Hypoxia is oxygen (oxia) insufficiency (hypo) at the tissue level, and a pulse oximetry reading of hypoxia is less than 70% (Bhutta et al., 2024).
A healthy adult should not have a saturation of less than 92%. This could indicate respiratory depression, obstruction (see Auscultation post), or disease (e.g., COPD and asthma).
Respiratory depression can occur from certain medications with sedative effects (e.g., propofol). This is why many protocols and monitors are in place when a person is being “put under” for surgery.
Chronic obstructive pulmonary disease (COPD) is an obstructive airway condition that restricts airflow. It is categorized into chronic bronchitis (inflammation of the bronchus) and emphysema (damaged alveoli). Patients with these disorders will have lower blood oxygen levels, and it may be challenging to take their saturation if they have clubbing (enlarged fingertips, a common symptom).
Asthma is similar in that it can cause airway inflammation and create extra mucus, making it difficult to get oxygen into the body. Having a patient with asthma take medication by inhalation (i.e., inhaler) before assessing them will increase their oxygen saturation and improve their lung sounds upon auscultation.
I learned a lot about these subjects while researching for this post. It is interesting to see the old uses of these everyday tools, like for athletes and pilots. What is the most interesting fact you learned in this post?
– V. A. Cyr
References
Barlocher, D. (2018). Polar's first coup: The Sport Tester PE2000 [Image]. https://www.galaxus.de/en/page/polar-the-forefather-of-the-heart-rate-monitor-in-retrospect-7430
Barlocher, D. (2018). One year later, the launch of the Tunturi Pulser [Image]. https://www.galaxus.de/en/page/polar-the-forefather-of-the-heart-rate-monitor-in-retrospect-7430
Bhutta, B.S., Alghoula, F. & Berim, I. (2024). Hypoxia. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482316/#
Billman, G. E. (2011). Heart rate variability - a historical perspective. Frontiers in Physiology, 2, 86. 10.3389/fphys.2011.00086
Brunner, M. (2020). Watson's Pulse Watch undefined [Image]. World Tempus. https://en.worldtempus.com/article/watches/trends-and-style/pulsometer-watches-how-fast-is-your-heart-beating-28441.html
Cables and Sensors. (n.d.). The History of Pulse Oximetry. https://www.cablesandsensors.com/pages/history-of-pulse-oximetry#:~:text=American%20inventor%20and%20physiologist%20Glenn,to%20oxygen%2Dstarved%20high%20altitudes.
Ceconi, C., Guardigli, G., Rizzo, P., Francolini, G., Ferrari, R. (2011). The heart rate story. European Heart Journal Supplements, 13, Supplemental C, C4–C13. https://doi.org/10.1093/eurheartj/sur014
Cosinuss. (n.d.). Fig. 4: Pulse measurement on the wrist with two fingers [Image]. https://www.cosinuss.com/en/measured-data/vital-signs/pulse-rate/
Curious Cyborg. (n.d.). The First Blood Oximeters [Image]. https://curiouscyborg.com/the-history-of-pulse-oximetry-measurement/
Curious Cyborg. (n.d.). Photograph of the Hewlett Packard Model 47201A Oximeter (LEFT) and the ear piece being applied to a patient (RIGHT) [Image]. https://curiouscyborg.com/the-history-of-pulse-oximetry-measurement/
Curious Cyborg. (n.d.). Photograph of the Nihon Kohden Pulse Oximeter OLV-5100 circa 1974, being demonstrated [Image]. https://curiouscyborg.com/the-history-of-pulse-oximetry-measurement/
India Mart. (n.d.). Portable Vital Signs Monitor [Image]. https://www.indiamart.com/proddetail/portable-vital-signs-monitor-13885477962.html
Jubran. (2015). Causes of inaccuracies. Open Critical Care. https://opencriticalcare.org/faq/what-does-a-normal-pulse-oximeter-photoplethysmograph-look-like/
King, L. M. (2024). What Is Heart Rate Variability? WebMD. https://www.webmd.com/heart/what-is-heart-rate-variability
Klabunde, R. E. (2023). SAN, sinoatrial node; AVN, atrioventricular node; RA, right atrium; LA, left atrium, RV, right ventricle; LV, left ventricle [Image]. Cardiovascular Physiology Concepts. https://cvphysiology.com/arrhythmias/a002
Konica Minolta. Minolta OXIMET MET-1471 [Image]. https://healthcare.konicaminolta.us/about-us/company-history
London Drugs. (n.d.). LifeSource Pulse Oximeter - UP-200CN [Image]. https://www.londondrugs.com/lifesource-pulse-oximeter---up-200cn/L1794533.htm
Mayo Clinic. (2023). Hypoxemia. https://www.mayoclinic.org/symptoms/hypoxemia/basics/definition/sym-20050930#:~:text=Hypoxemia%20is%20a%20low%20level,to%20breathing%20or%20blood%20flow.
Mendelson, Y. (2017). Soon thereafter, Biox Technology and Nellcor commercialized a similar finger pulse oximeter by taking advantage of advancements in semiconductor technology. [Image]. http://dx.doi.org/10.13028/wy2t-dn34
Merriam-Webster. (n.d.). Pulse Definition & Meaning. https://www.merriam-webster.com/dictionary/pulse
Mount Sinai. (2024). Electrocardiogram [Image]. https://www.mountsinai.org/health-library/tests/electrocardiogram
Mount Sinai. (n.d.). Hemoglobin [Image]. https://www.mountsinai.org/health-library/tests/hemoglobin
National Heart, Lung, and Blood Institute (NHLBI). (2022). How the Heart Works: How the Heart Beats. National Institute of Health. https://www.nhlbi.nih.gov/health/heart/heart-beats#:~:text=Your%20heart%20has%20a%20special,to%20contract%20and%20pump%20blood.
Peterson, B. K. (2007). Chapter 22 - Vital Signs. In M. H. Cameron & L. G. Monroe’s Physical Rehabilitation. W.B. Saunders. 598-624. https://doi.org/10.1016/B978-072160361-2.50025-9
Pickering, D. (2013). How to measure the pulse. Community Eye Health, 26(82), 37. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3756652/
Plaza, J. V. (2023). Table prepared by Joaquín Vico Plaza, Vitruve editor. HRR: heart rate reserve; bpm: beats per minute [Image]. Vitruve. https://vitruve.fit/blog/frequency-of-heart-rate-at-rest-in-athletes-according-to-age-and-gender/
Radiology Buzz. (5 July, 2020). About Heart Beat, Normal, Bradycardia and Techy cardia [Video]. YouTube. https://www.youtube.com/watch?v=BhJ93a9fSlk
Saki, N. & Bandar, B. (2023). Hemoglobin C Crystals [Image]. American Society of Hematology Image Bank. https://imagebank.hematology.org/image/64586/hemoglobin-c-crystals
Tarnoki, A. D., Szalontai, L., Fagnani, C., Tarnoki, D. L., Lucatelli, P., Maurovich-Horvat, P., Jermendy, A. L., Kovacs, A., Molnar, A. A., Godor, E., Fejer, B., Hernyes, A., Cirelli, C., Fanelli, F., Farina, F., Baracchini, C., Meneghetti, G., Gyarmathy, A. V., Jermendy, G., Merkely, B., Pucci, G., Schillaci, G., Stazi, M. A. & Medda, E. (2021). Genetic and environmental factors on heart rate, mean arterial pressure and carotid intima-media thickness: A longitudinal twin study. Cardiology Journal, 28(3), 431-438. 10.5603/CJ.a2019.0089
Terry, S. (2024). Pulse measurement, 14th century artwork [Image]. Media Storehouse.https://www.mediastorehouse.com.au/science-photo-library/pulse-measurement-14th-century-artwork-6419945.html
Torp, K. D., Modi, P., Pollard, E. J. & Simon, L. V. (2023). Pulse Oximetry. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK470348/#
Tri-anim. (n.d.). OxiMax Pulse Oximeter Sensors [Image]. https://www.tri-anim.com/ths/diagnostics-monitoring/pulse-ox-sensors-probes/oximax-pulse-oximeter-sensors/p/group002980
Wikipedia. (2024). Heart rate monitor. https://en.wikipedia.org/wiki/Heart_rate_monitor

Comments